COVID-19 impact on life expectancy among municipalities of Northeastern states of Mexico
DOI:
https://doi.org/10.29059/cienciauat.v18i1.1765Keywords:
COVID-19, mortality, life expectancy, municipalities, Northeastern MexicoAbstract
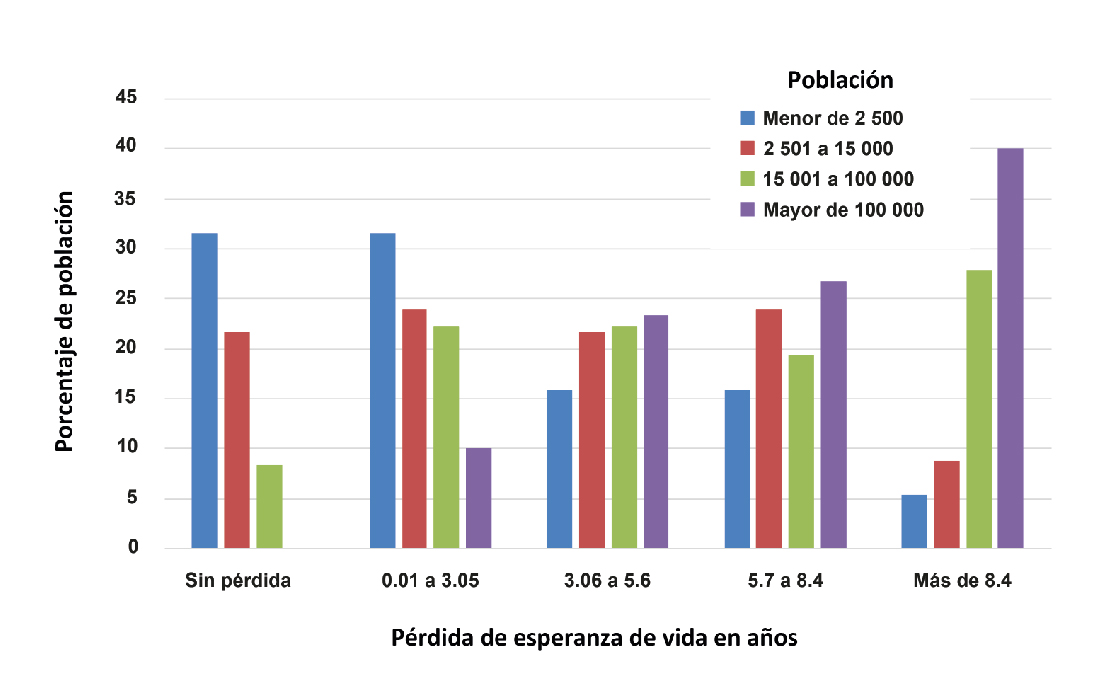
COVID-19 mortality in Mexico is among the highest in the world. Therefore, it is of epidemiologic interest to study its impact on life expectancy. The aim of the present paper was to analyze the impact of the COVID-19 pandemic on life expectancy through a comparison of data from 2019 and 2020. Specifically, the effect of population density in municipalities of Northeastern Mexican states. Information regarding 2019 and 2020 mortality rates for was obtained from the Ministry of Health, and demographics from the National Population Council. Life tables were constructed using the standard actuarial method. Percentiles ≤ 25 and ≥ 75 of the difference in life expectancy in the period were calculated. The relationship between the size of the population of the municipalities and the magnitude of the difference in life expectancy loss of years was evaluated. COVID-19 pandemic impacted on life expectancy with great heterogeneity in each of the northeastern states of Mexico. The loss in years in average life expectancy was 5.4 for Coahuila, 4.1 for Nuevo Leon and 4.9 for Tamaulipas. Municipalities above the ≥ 75th percentile showed an average loss of 9.2 years. Those in the lower than ≤ 25th percentile showed a decrease, of -0.35 years. The difference in the loss of life expectancy during 2019 and 2020 was influenced by population size, tending to be greater in those municipalities with higher population density, but was not the only determining factor.
References
Aburto, J. M., Schöley, J., Kashnitsky, I., Zhang, L., Rahal, C., Missov, T. I., ..., and Kashyap, R. (2022). Quantifying impacts of the COVID-19 pandemic through life-expectancy losses: a population-level study of 29 countries. International Journal of Epidemiology. 51(1): 63–74. DOI: https://doi.org/10.1093/ije/dyab207
Andrasfay, T. and Goldman, N. (2022). Reductions in US life expectancy during the COVID-19 pandemic by race and ethnicity: Is 2021 a repetition of 2020? Plos One. 17(8): e0272973. DOI: https://doi.org/10.1371/journal.pone.0272973
Arias, E. (2004). National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. United States Life Tables. 52(14): 1–38.
Bhadra, A., Mukherjee1, A, and Sarkar, K. (2021). Impact of population density on Covid 19 infected and mortality rate in India. Modeling Earth Systems and Environment. 7: 623–629. DOI: https://doi.org/10.1007/s40808-020-00984-7
Bonnet, F., Grigoriev, P., Sauerberg, M., Alliger, I., Mühlichen M., and Carlo-Giovanni, C. (2023). Spatial variation in excess mortality across Europe: a crosssectional study of 561 regions in 21 countries, in Med Rxiv preprint. [En línea]. Disponible en: https://doi.org/10.1101/2023.04.04.23284990. Fecha de consulta: 2 de junio de 2023. DOI: https://doi.org/10.1007/s44197-024-00200-0
Cervera-Flores, M. y Rangel-González, J. W. (2015). Distribución de la población por tamaño de la localidad y su relación con el medio ambiente. [En línea]. Disponible en: https://www.inegi.org.mx/eventos/2015/poblacion/doc/p-walterrangel.pdf. Fecha de consulta: 13 de julio de 2022.
CONAPO, Consejo Nacional de Población (2018). Proyecciones de la población de México y de las entidades federativas, 2016–2050, Documento metodológico. México: Secretaría de Gobernación, CONAPO,
UNFPA. [En línea]. Disponible en: https://www.gob.mx/cms/uploads/attachment/file/390959/Proyecciones_de_la_poblacion_de_Mexico_2016_2050_primera_parte.pdf. Fecha de consulta: 15 de julio de 2022.
CONEVAL, Consejo Nacional de Evaluación de la Política Pública de Desarrollo Social (2019). La pobreza en la población indígena de México, 2008-2018. [En línea]. Disponible en: https://www.coneval.org.mx/Medicion/MP/Documents/Pobreza_Poblacion_indigena_2008-2018.pdf. Fecha de consulta: 14 de julio de 2022.
Cuéllar, L., Torres, I., Romero-Severson, E., Mahesh, R., Ortega, N., Pungitore, S., …, and Ke, R. (2022). Excess deaths reveal the true spatial, temporal and demographic impact of COVID-19 on mortality in Ecuador. International Journal of Epidemiology. 51(1): 54-62. DOI: https://doi.org/10.1093/ije/dyab163
Cutler, D., Deaton, A., and Lleras-Muney, A. (2006). The determinants of mortality. Journal of Economic Perspectives. 20(3): 97-120. DOI: https://doi.org/10.1257/jep.20.3.97
García-Guerrero, V. M. y Beltrán-Sánchez, H. (2021). Heterogeneity in excess mortality and its impact on loss of life expectancy due to covid-19: Evidence from Mexico. Canadian Studies in Population. 48(2): 165-200. DOI: https://doi.org/10.1007/s42650-021-00051-1
Hernández-Bringas, H. (2020). Covid-19 en México: Un perfil sociodemográfico. Notas de Población. (111): 105-132. DOI: https://doi.org/10.18356/16810333-47-111-6
Hyndman, M. R. J., Booth, H., Tickle, L., and Maindonald, J. (2019). Package ‘demography’, v. 1.22. [En línea]. Disponible en: https://cran.r-project.org/web/packages/demography/demography.pdf. Fecha de consulta: 19 de julio de 2022.
INEGI, Instituto Nacional de Información Estadística y Geografía (2021). Estadísticas a propósito del día mundial de la diabetes. Datos Nacionales, en Comunicado de prensa 645/21. [En línea]. Disponible en: https://www.inegi.org.mx/contenidos/saladeprensa/aproposito/2021/EAP_Diabetes2021.pdf. Fecha de consulta: 8 de julio de 2022.
Islam, N., Jdanov, D. A., Shkolnikov, V. M., Khunti, K., Kawachi, I., White, M., ..., and Lacey, B. (2021). Effects of covid-19 pandemic on life expectancy and premature mortality in 2020: time series analysis in 37 countries. BMJ (Clinical Research). 375: e066768. DOI: https://doi.org/10.1136/bmj-2021-066768
Juárez-Rendón, K. J. y Parra-Bracamonte, G. M. (2022). Características y factores de riesgo de mortalidad por COVID-19 en Tamaulipas, a un año de pandemia. CienciaUAT. 17(1): 6-16. DOI: https://doi.org/10.29059/cienciauat.v17i1.1652
Lara-Rivera, A. L, Parra-Bracamonte, G. M, López-Villalobos, N. (2021). Tasas de letalidad y factores de riesgo por COVID-19 en México. Revista Cubana de Salud Pública. 47(4): e2872.
Leon, D. A., Shkolnikov, V. M., Smeeth, L., Magnus, P., Pechholdová, M., and Jarvis, C. I. (2020). COVID-19: a need for real-time monitoring of weekly excess deaths. The Lancet. 395(10234): e81. DOI: https://doi.org/10.1016/S0140-6736(20)30933-8
Lima, E. E., Vilela, E. A., Peralta, A., Rocha, M., Queiroz, B. L., Gonzaga, M. R., ..., and Freire, F. H. (2021). Investigating regional excess mortality during 2020 COVID-19 pandemic in selected Latin American countries. Genus. 77(1): 1-20. DOI: https://doi.org/10.1186/s41118-021-00139-1
Lui, B., Zheng, M., Robert, S., White, R. S., and Hoyler, M. (2021). Economic burden of lives lost due to COVID-19 in New York Stat. Journal of Comparative Effectiveness Research. 10(11): 893-897. DOI: https://doi.org/10.2217/cer-2021-0086
Martínez, R., Soliz, P., Caixeta, R. y Ordunez, P. (2019). Reflexión sobre métodos modernos: años de vida perdidos por mortalidad prematura: una medida versátil e integral para monitorear la mortalidad por enfermedades no transmisibles. Int J Epidemiol. 48(4): 1367-1376.
McCartney, G., Leyland, A., Walsh, D., and Ruth, D. (2021). Scaling COVID-19 against inequalities: should the policy response consistently match the mortality challenge? J Epidemiol Community Health. 75(4): 315-320. DOI: https://doi.org/10.1136/jech-2020-214373
Mena, G. and Aburto, J. M. (2022). Unequal impact of the Covid-19 pandemic in 2020 of life expectancy across urban areas in Chile: A crosssectional demographic study. BMJ Open. 12(8): e059201. DOI: https://doi.org/10.1136/bmjopen-2021-059201
Núñez-Medina, G. (2021). Análisis espacio-temporal de la tasa de letalidad por coronavirus dada la preexistencia de diabetes en los municipios del noreste de México. Espacio Abierto. 30(2): 87-99.
OPS, Organización Panamericana de la Salud (2015). Glosario de indicadores básicos de la OPS. [En línea]. Disponible en: https://www.paho.org/es/documentos/glosario-indicadores-basicos-ops. Fecha de consulta: 8 de julio de 2022.
Palacio-Mejía, L. S., Hernández-Ávila, J. E., Hernández-Ávila, M., Dyer-Leal, D., Barranco, A., Quezada-Sánchez, A. D., ..., and López-Gatell, H. (2022). Leading causes of excess mortality in Mexico during the COVID-19 pandemic 2020-2021: A death certificates study in a middle-income country. Lancet Regional Health. Americas. 13: 100303. DOI: https://doi.org/10.1016/j.lana.2022.100303
Parra-Bracamonte, G. M., Lopez-Villalobos, N., and Parra-Bracamonte, F. E. (2020). Clinical characteristics and risk factors for mortality of patients with COVID-19 in a large data set from Mexico. Ann Epidemiol. 52: 93-98. DOI: https://doi.org/10.1016/j.annepidem.2020.08.005
Parra-Bracamonte, G. M., Parra-Bracamonte, F. E., Lopez-Villalobos, N., and Lara-Rivera, A. L. (2021). Chronic kidney disease is a very significant comorbidity for high risk of death in patients with COVID-19 in Mexico. Nephrology. 26(3): 248-251. DOI: https://doi.org/10.1111/nep.13827
Pierce, J. B., Harrington, K., McCabe, M. E., Petito, L. C., Kershaw, K. N., Pool, L. R., ..., and Khan, S. S. (2021). Racial/ethnic minority and neighborhood disadvantage leads to disproportionate mortality burden and years of potential life lost due to COVID-19 in Chicago, Illinois. Health & Place. 68: 102540. DOI: https://doi.org/10.1016/j.healthplace.2021.102540
PNUD, Programa de las Naciones Unidas para el Desarrollo (2015). Índice de desarrollo humano para las entidades federativas, México 2015: Avance continuo, diferencias persistentes. [En línea]. Disponible en: http://pued.unam.mx/export/sites/default/archivos/SUCS/2015/180215RTG.pdf. Fecha de consulta: 3 de agosto de 2022.
Raleigh, V. (2019). Trends in life expectancy in EU and other OECD countries: Why are improvements slowing?, in OECD Health Working Papers, No. 108. [En línea]. Disponible en: https://www.oecd-ilibrary.org/social-issues-migration-health/trends-in-life-expectancy-in-eu-and-other-oecd-countries_223159ab-en. Fecha de consulta: 25 de julio de 2022.
Rojo-del-Moral, O. (2022). Mortalidad de pacientes infectados por infección por SARS-CoV-2 en México. Análisis de una base de datos nacional a dos años de la pandemia. Gaceta Médica de México. 158: 425-431. DOI: https://doi.org/10.24875/GMM.22000253
Roy-García, I., Rivas-Ruiz, R., Pérez-Rodríguez, M. y Palacios-Cruz, L. (2019). Correlación: no toda correlación implica causalidad. Revista Alergia México. 66(3): 354-360. DOI: https://doi.org/10.29262/ram.v66i3.651
Salinas-Aguirre, J. E., Sánchez-García, C., Rodríguez-Sanchez, R., Rodríguez-Muñoz, L., Díaz-Castaño, A. y Bernal-Gómez, R. (2022). Características clínicas y comorbilidades asociadas a mortalidad en pacientes con COVID-19 en Coahuila (México) [Clinical characteristics and comorbidities associated with mortality in patients with COVID-19 in Coahuila (Mexico)]. Revista Clinica Espanola. 222(5): 288–292. DOI: https://doi.org/10.1016/j.rce.2020.12.006
SS, Secretaría de Salud (2020). Datos Abiertos. [En línea]. Disponible en: https://www.gob.mx/salud/documentos/datos-abiertos-152127. Fecha de consulta: 24 de julio de 2022.
Team R Core (2016). R: A Language and Environment for Statistical Computing, in Vienna: R Foundation for Statistical Computing. [En línea]. Disponible en: https://www.R-project.org/. Fecha de consulta: 28 de julio de 2022.
Trias-Llimós, S., Riffe, T., and Bilal, U. (2020). Monitoring life expectancy levels during the COVID-19 pandemic: Example of the unequal impact of the first wave on Spanish regions. PloS One. 15(11): e0241952. DOI: https://doi.org/10.1371/journal.pone.0241952
Wang, H., Paulson, K. R., Pease, S. A., Watson, S., Comfort, H., Zheng, P., ..., and Murray, C. J. (2022). Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. The Lancet. 399(10334): 1513-1536.
Worldometer (2022). Covid-19 coronavirus pandemic: Coronavirus Upday. [En línea]. Disponible en: https://www.worldometers.info/coronavirus/. Fecha de consulta: 24 de julio de 2022.
WHO, World Health Organization (2020). Pneumonia of unknown cause – China. Covid-19-China. [En línea]. Disponible en: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/. Fecha de consulta: 6 de julio de 2022.
Xu, J. J., Chen, J. T., Belin, T. R., Brookmeyer, R. S., Suchard, M. A., and Ramirez, C. M. (2021). Racial and Ethnic Disparities in Years of Potential Life Lost Attributable to COVID-19 in the United States: An Analysis of 45 States and the District of Columbia. International Journal of Environmental Research and Public Health. 18(6): 2921. DOI: https://doi.org/10.3390/ijerph18062921
Yadav, S., Yadav, P. K., and Yadav, N. (2021). Impact of COVID-19 on life expectancy at birth in India: a decomposition analysis. BMC Public Health. 21(1): 1906. DOI: https://doi.org/10.1186/s12889-021-11690-z
Published
How to Cite
License
Copyright (c) 2022 Universidad Autónoma de Tamaulipas

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Accepted 2023-07-06
Published 2023-07-20